A WhatsApp message claiming that humidity caused due to use of masks causes Mucormycosis (black fungus) is misleading. Experts highlight that people with poorly managed diabetes and a weak immune system are at a high risk of mucormycosis.
By Pushpita Dey
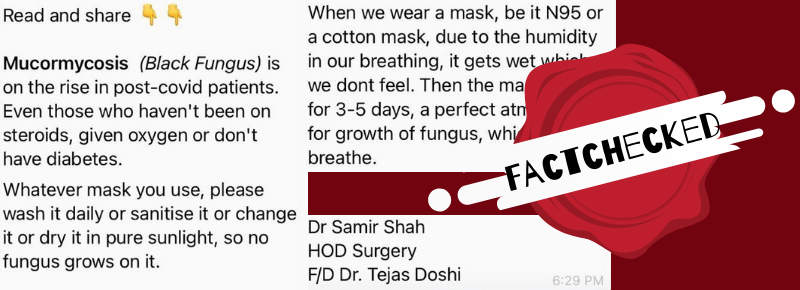
Recently, a message is being widely circulated on Whatsapp that claims “when we wear a mask, be it N95 or a cotton mask, due to the humidity in our breathing, it gets wet which we don’t feel. Then the mask is used for 3-5 days, a perfect atmosphere for the growth of fungus(Mucormycosis/Black fungus), which we breathe.”
The claim in the message is misleading.
The screenshot of the circulated message has been attached below.

The message was attributed to some Dr. Samir Shah. Since the name of the hospital was not given, keyword search for Dr. Samir Shah didn’t yield many results in the field of surgery. Even after an advanced search, we couldn’t connect with him as there were no credentials.
To verify the claim in the message, we contacted Dr. Dulal Bose, an ENT specialist and clinical director of Peerless Hospital, Kolkata, who has done extensive academic research on Mucormycosis. Talking about the spread of the fungus, he mentioned that, “It is always advisable to wash the (cotton) mask well and dry them under sunlight to clean them. But the cases of Mucormycosis is nothing new in India, and we have also got quite a few cases even before the COVID outbreak or the use of masks.”
Dr. Sanjeev Kumar, Associate Professor, CFM Department, AIIMS Bhopal explained, “if high humidity has been the sole cause, then places like Cherapunji and Kolkata, where the humidity is very high, would have a very high number of cases of Mucormycosis. But no such reports are known till now.”
Dr. Manojendra Narayan Bhattacharyya, Senior Consultant ENT Head & Neck Surgeon, Fortis Hospital, Kolkata, said “steroids usage should be monitored and used judiciously. Unmonitored usage of steroids leads to an environment of immuno-suppression”.
But the question is why there has been an increase in the number of cases reported of Mucormycosis, specifically after the COVID second wave.
Talking about if there is any role of COVID in the growth of Mucormycosis, Dr. Bose clarified, “Even before the pandemic, various cases of Mucormycosis were reported in western India. But during the first wave, a number of cases of mucormycosis were reported as such. But now, the new variant of the virus has become so virulent in some of the patients’ bodies that it badly affects body immunity. Lack of body immunity makes it easy for the fungus to invade the body.”
Agreeing to this, Dr. Manojendra Narayan Bhattacharyya mentioned, “Fungus including Mucormycosis is the most opportunistic microbe. Under any immuno-compromised situation in a body, that may be due to diabetes, cancer, nutrient deficiency etc., it can attack either through the nose or through any wounded area exposed to the air.” According to reports of the National Center for Biotechnology Information Mucormycosis occurs in patients who are immunocompromised because of diabetic ketoacidosis, neutropenia, organ transplantation, and/or increased serum levels of available iron.
Dr. Sanjeev Kumar further added, “it is known from the previous medical literature that use of prolonged antibiotics along with high dose steroids are linked with the development of Mucormycosis."
It has also been pointed out by the doctors that unhygienic conditions like improper sanitation of oxygen delivery masks, inappropriate medications from unqualified medical practitioners have led to the attack of Mucormycosis in many patients.
Dr. Manojendra Narayan Bhattacharyya strictly advises against washing or sanitising N-95 or surgical masks using sanitisers. “They should be disposed of”.
Johns Hopkins Medicine provides tips on using and cleaning a variety of different face masks here.