Latest
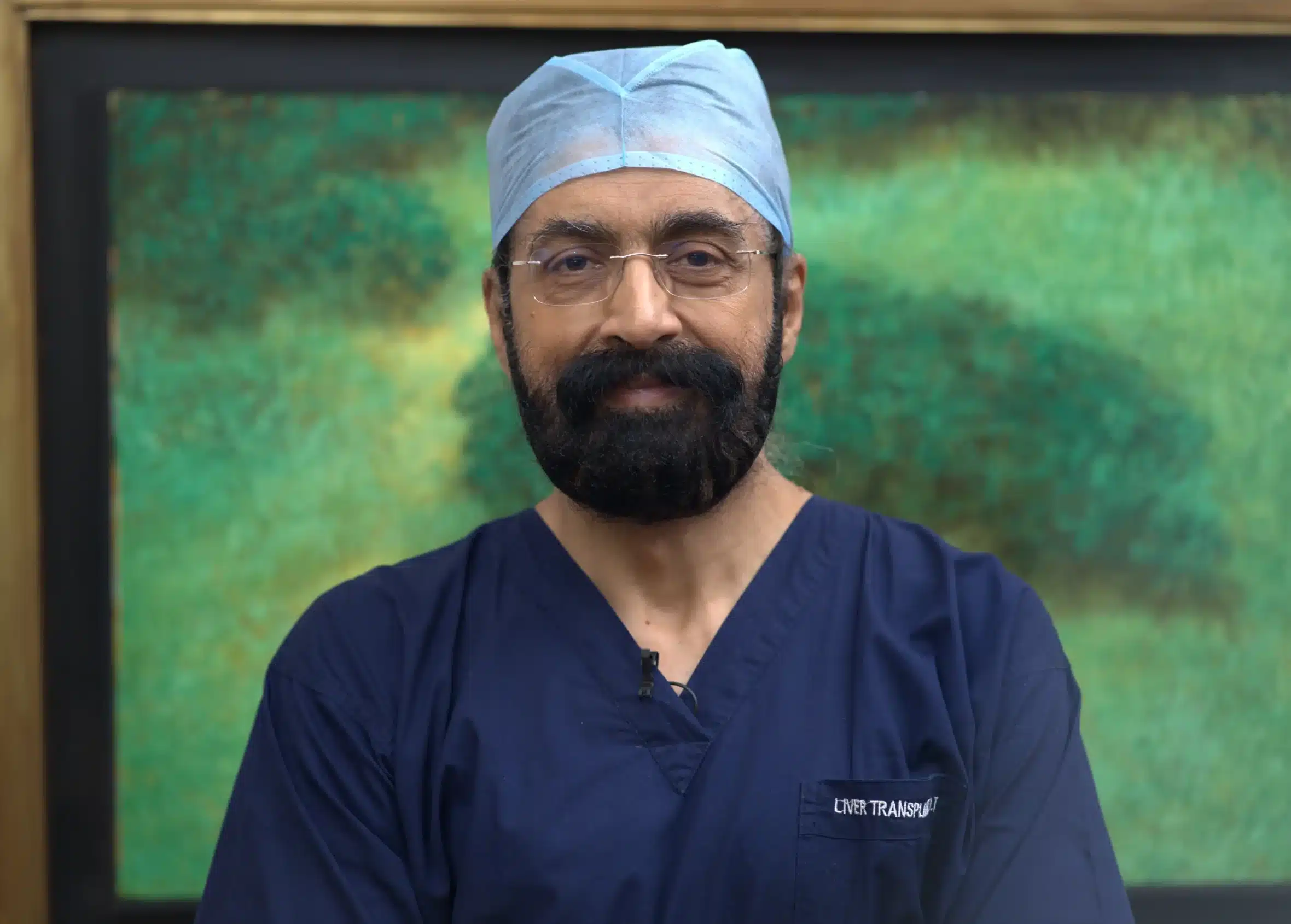
World Organ Donation Day: ‘Don’t take your organs to heaven; heaven knows we need them here,’ says leading liver transplant surgeon Dr Arvinder Singh Soin
The push for organ donation has never been stronger — but awareness is still our biggest challenge, according to Dr Soin who performed the country’s first liver transplant surgery almost 3 decades ago.
Author
Author
- admin / 4 months

- 0
- 16 min read

Author
According to the Union Health Ministry, India has made unprecedented progress in the field of organ transplantation — performing over 18,900 organ transplants in 2024 alone, the highest ever recorded in a single year. This is a sharp rise from fewer than 5,000 such surgeries in 2013, placing India third in the world after the United States and China. Yet, despite this remarkable growth, the gap between the demand for donor organs and their availability remains daunting — every year, 2.5 lakh people require kidneys, 1 lakh need corneas, 80,000 require livers, and 50,000 need hearts.
This World Organ Donation Day, we spoke to Dr Arvinder Singh Soin, the pioneer of liver transplantation in India who performed the first ever liver transplant in India and has since performed close to 5,000 liver transplants, on the current state of organ donation in the country, the challenges in bridging the demand-supply gap, and how to overcome myths and misinformation that prevent people from becoming donors.
Here are the excerpts from that conversation:
Mariyam Alavi (for First Check): I was reading about your work, and it really is inspiring. You were the first person to do a liver transplant surgery in the country in 1998. So, tell me about that. How was that? Because I can imagine it being a slightly crazy conversation trying to convince a patient to put in somebody else’s organ into their body, and to do that for the first time ever in the country. How did that play out?
Dr Arvinder Singh Soin: You know, so I was at Cambridge University for six and a half years before that. And I was routinely doing liver transplants, kidney transplants, pancreas transplants from deceased donor organs. These are basically donors who die of brain death, and their next of kin agrees to donate organs. So that was pretty routine back in the UK when I was at Cambridge.
And then I started transplantation in Delhi, at the Apollo Hospital. So when we got going a few months down the line, we prepared everything. And then on the 5th and 6th November night, we had a brain-dead person in the ICU within the same hospital. And we spoke with them because somebody in their family had donated eyes earlier. And eye donation is a little different from brain dead organ donation because eye donation can be done by anyone, dying any kind of death at home, on the road, etc., or in the hospital. But brain-dead persons donating organs only happens in neuro-ICUs in a hospital where they are brain dead and the other organs are functioning. The other organs are kept going on a ventilator and other ICU support. So that kind of situation is different and it only happens in 1% of the deaths.
So on November 5th evening, we got to know of such a person and they had expressed a wish to actually donate organs, just because somebody in their family had donated eyes earlier (Corneas). So back in the UK, I had a system where there were transplant coordinators, there were counsellors who actually spoke to such families. But in my hospital in Delhi, this was very new to everyone. There was no system or team to actually make that happen. I and my colleague surgeon, we actually counselled this family and they agreed to donate organs.
Of course, the Organ Donation Act was in place. So the documentation was possible. And obviously, any modern ICU could declare brain death. The procedure, although hadn’t been done before, was not undoable. So it was possible to do it.
The family, luckily, because they had been primed by a previous donation in their own family, they agreed to donate organs. And then we had two patients on the waiting list and we spoke to each one of them whether they would have that organ. And one of them actually agreed, because he was told that he didn’t have more than 2 or 3 months to live if he didn’t actually have a liver transplant. And I also told him that, ‘look, it’s very new for this country. This is the first case in this country. But I’ve done hundreds in UK and this was pretty routine to save patients from dying of liver failure with liver transplants. And this is the only shot you’ve got. So why don’t you agree?’
So he and his family agreed and we went ahead with the country’s first deceased donor liver transplant on the night of 5th, 6th November, 1998. And the patient did well. We discharged him 13 days after transplant and that was the first successful transplant of this country.
And so in terms of the surgical challenge, there wasn’t much because I had done lots of these procedures earlier. But the system wasn’t geared up completely. So we had to do the counseling. No surgeon does counseling nowadays for families. There are separate transplant coordinators and grief counselors that do that. We had to do it. And then, of course, we did the surgery. We had to take care of the patient in the ICU afterwards. So in that way, of course, the system wasn’t that geared up and we had to do everything. And that in itself was a unique experience and a challenge. But it worked out well. And that really got things going in India as far as transplantation is concerned.
But now almost three decades later, and you’ve now done close to 5,000 transplant surgeries, what has changed since that first surgery that you did and how it goes about right now?
Lots has changed. So that was the first case was a deceased donor of a transplant, which means the organ came from a brain-dead person. But brain-dead donors do not account for more than 20%- 25% transplants in this country. So the majority of the transplants still happen with living donors. And I’m talking only about liver transplants. So in liver transplants and in kidney transplants, living donation accounts for between 80% and 90% of the transplants that are done in this country. So just like you said, you think 80,000 people need liver transplants. That’s absolutely true. But we only have just about 1,000 brain-dead donors in the entire country.
So the figure of 18,000 or 19,000 organ transplants you said was actually including the corneal transplants, the eye transplants. So if you leave them out, because I already told you that’s different, because that can happen from any dead person, then if you just consider the organs that are transplanted from a brain-dead person, there were about 3,500 of them done last year and about 3,000 done in 2023. And the number of brain-dead donors that we had last year was about 1,100 and the number we had in 2023 was just 1,000.
1,000 brain-dead donors in a country of 1.4 billion people. That’s way too low, right? So that gives you a donation rate of about 0.6, 0.7 per million. And to give you context, the donation rates in Spain are about 58 per million, in the UK are about 30 per million, in the US are about 50 per million. And we are just at about 0.7/ 0.8 per million.
But why do you think that’s still an issue here? I mean, we are a big country, we have a huge population. One would expect our pool of donors to also be huge. But why do we still have reluctance when it comes to organ donation?
There are several reasons for that. And one of the main reasons is that the awareness for organ donation is still not where it needs to be. In the sense that now for the last about 10 years, the government has been doing a lot of active work in organ donation, in promotion of organ donation, and spreading the awareness across the country, across every section of society. But it wasn’t so much prevalent before that. Although the act that allows organ donation from brain-dead donors and also from the living donors has been there for over 40 years, 1984, right? But it’s organ donation in terms of brain death and then people donating organs is only picking up now for the last five or seven years. So one is awareness.
And two is, of course, expertise for retrieving organs. But I believe that’s not the bottleneck right now, it’s just awareness.
And, you know, people have variously held beliefs that they shouldn’t be removing organs from their loved ones who die of brain death because, you know, they may not have the same organs the next time around when they’re born. Or people haven’t understood what brain death is because in brain-dead people, I told you they’re on ventilators and they’re on life support. So even though the brain is dead, there is perception of life because if you look at the monitor, the heart is still going, there is a BP. So not everyone understands that such a person is actually dead. So even though obviously the ICU counsellors and doctors explain this concept to the relatives but not everyone’s able to comprehend it, right? So they refuse organ donation. So that’s the second part. They don’t believe that their loved one is gone. Or there is this myth about, you know, the organs that are donated will not be there the next time.
So these are just two of the myths. Then there is a myth that people think that their religion doesn’t allow it. Now there is no actual mainstream religion that does not allow it. But it’s just people’s beliefs and myths. So I think that a lot of work still has to be done because as the donation rates are less than 1 per million and we really have to reach at least 10-15 per million to have a sizable number of donors and increase the number of transplants.
A couple of interesting things there. But first, I just want to talk to you about the kind of misinformation and lack of awareness that you talked about. Have you had to deal with this personally as well in your career? When you’ve had to counsel or talk to people about these sorts of strongly held beliefs.
We don’t do that anymore. I told you that surgeons have no role now in counseling families who will be saying yes for their loved ones to donate. That is done by a specialist called transplant coordinators and grief counselors. And that is done by the ICU team. By protocol, the transplant team never interacts with the family anymore. It wasn’t supposed to even when I did the first case but there was nobody else to do it. So that’s why we did it.
But the answer is yes. The transplant coordinators and people that counsel families face this every day.
So there is an additional element of commerce. Which means that a lot of families think that hospitals will sell organs and make money out of them. But there’s nothing like that. Because every transplant is very heavily regulated. Every patient’s detail is submitted to the ministry soon after the transplant. What happened to the patient is submitted to the ministry. So everything is under a very fine lens. There is never any misallocation of organs as far as deceased donor organs are concerned. But there is a perception in some people’s minds. So these are all the reasons why organ donations are refused.
In fact, a couple of days back, our health minister, Mr J.P. Nadda, said that there has been an increase in organ failures. Because of which, our need for organs has also risen over the past couple of years. Have you seen that in your career as well? Are we looking for more donors?
The need for donor organs have risen. That is correct. And as far as liver failure is concerned and liver transplants go. Yes, we have seen a rise in end-stage liver disease, liver failure, liver cancer. These are the reasons why people need liver transplants.
And that has gone up and largely because of what we call MASLD- Metabolic Dysfunction Associated Steatotic Liver Disease. So metabolic dysfunction means basically fatty liver disease. What used to be called NAFLD, non-alcoholic fatty liver disease. That means people who don’t even have alcohol but have uncontrolled diabetes, have bad lipids and cholesterol or are overweight or have bad lifestyle. They could basically get liver failure and that is the leading cause of liver failure now.
In India, 4 out of every 10 adults actually have a fatty liver. And as many as 10-15% of them can develop serious liver disease if they don’t control this in time. So yes, that’s the reason. The NAFLD or now rechristened as MASLD is the new scourge as far as liver diseases go.
Check)
So you’ve said that you’ve seen this increase in liver disease. So has there been a corresponding increase in donor organs or transplant surgeries as well?
So transplant surgery is rising. Now in India we do approximately 5000 liver transplants a year. Which is the second highest in the world. The highest are done in the US at about 10,000 something. And now we are second with 5000. But like I said, majority of those transplants are living donor transplants.
So last year we did about 1000 liver transplants from deceased donors. And about 4000 from living donors. But this number needs to rise at least 15 to 20 times.
So that’s the degree of increase that is needed. But then yes, if you consider that in 1998 we did just one transplant in the country. That was one that I did. And then slowly the number has actually risen from a few to hundreds to thousands and it’s reached this number of 5000. And I’m sure maybe in the next 5 years we’ll see about 15K to 20K liver transplants a year.
How do we ensure that that happens? How do we encourage more people to donate organs? How do we help bridge that gap?
So like I said, spreading awareness. And how do you spread that awareness? It has to be the state that does it. Any number of NGOs and hospitals and doctors and you and I can keep talking about it. But it’s not going to happen as a movement nationally. Unless the government or the state governments and the central government give it a huge push. And they are. Let’s be honest and fair. The push for organ donation has never been more… And the push needs to continue until we achieve the donation rates that we need.
Now, some of the ways in which awareness can be spread. Majority of the states now have a box where you have to tick whether you want to be an organ donor when you get your (driver’s) license. That wasn’t the case five years ago. This has just happened in 2017-18 onwards, so that’s a big step forward.
Now, there is inclusion of the concept of brain death and organ donation in school textbooks. So you have to get this whole information percolating down to society at the kid level. So that, you know, when they grow up, they have already imbibed the concept of organ donation.
So I think it’s a slow process, but it’s happening. And then there should be some, SOPs, so to speak, given to people who donate organs. Or, for example, if I donate my loved one’s organs, then, I get some health insurance or, you know, something like that. So those kind of things have to be built in. You can’t actually give financial incentives to people donating organs. That never happens. No society, no transplant community agrees with that. But there should be some benefits given to the families of organ donors. So that’s another way you can do it.
And then this conversation needs to happen at the religious leaders’ level as well. You know, people listen to their religious leaders. And frank conversations where every religion encourages organ donation have to happen whenever there are discourses happening in any religion.
So then the other way to push organ donation is law allows you to declare brain death whenever doctors are doing rounds in ICUs and they find someone, maybe brain dead, you know, because they can suspect it clinically. Then you are allowed to, in fact, it’s mandatory to examine that patient and see if they are brain dead. So this is called mandatory declaration of brain death. And that’s law. But still majority of the hospitals don’t follow it. Because if that was to happen, then the identification of potential brain dead donors would increase.
And then there is a thing called required request, which means that if somebody is brain dead in an ICU, you have to ask their next of kin for organ donation. So if these two things are practised in every hospital that has an ICU, where such patients are admitted, organ donation rates will definitely rise.
Then there is this concept of a champion. Often in hospitals or even in government departments, there are health officials and in hospitals there are intensivists, there are grief counselors who want to champion the cause of organ donation. You know, they feel proud that they are able to convert some families to agree to organ donation so they can save lives.
And people should not misunderstand this. This is not about taking organs from people who can be otherwise saved. This is only from people who are dead, but by brain death. Because brain death is a mode of dying. So when somebody is brain dead, they are dead. They’re not in coma, they can’t wake up. So that’s for sure, people need to understand the concept. People who are working for this cause have to be rewarded for their work in increasing organ donation, saving lives.
Thank you so much, Dr Soin, for your time, but before we wrap up, if there is one advice or one message that you would have for our audience, what would that be?
The gift of life is the greatest gift of all. Please don’t take your organs to heaven. Heaven knows we need them here.
With inputs from Sakshi Srivastava
Also Read: World Organ Donation Day: Here’s what you need to know










