Explained | Why men’s fertility declines with age and what to do
Understanding how age affects sperm quality, testosterone levels, and reproductive outcomes is essential, not just for conception but also for the health of offspring and maternal outcomes
Author
Author
- admin / 2 months

- 0
- 9 min read

Author
For years now, women have been warned of their ticking biological clock. It has become almost routine to see reels, posts, and articles reminding women that their fertility peaks in their twenties and starts declining sharply after the mid-thirties. By the late thirties and early forties, the so-called “bell” of the female biological clock tolls louder, urging timely decisions about conception. Elders in Indian families, and others as well, push women to “settle down” before it’s too late, citing this self-imposed timeline.
While this message is repeated constantly in popular media, around dinner tables, and in most households, the male biological clock is far less discussed. After all, men like Al Pacino, Robert De Niro and Mick Jagger have fathered children well into their seventies and eighties. It almost seems as if men are exempt from fertility concerns. But emerging research shows that male fertility is not immune to ageing, and understanding this can be crucial for family planning.
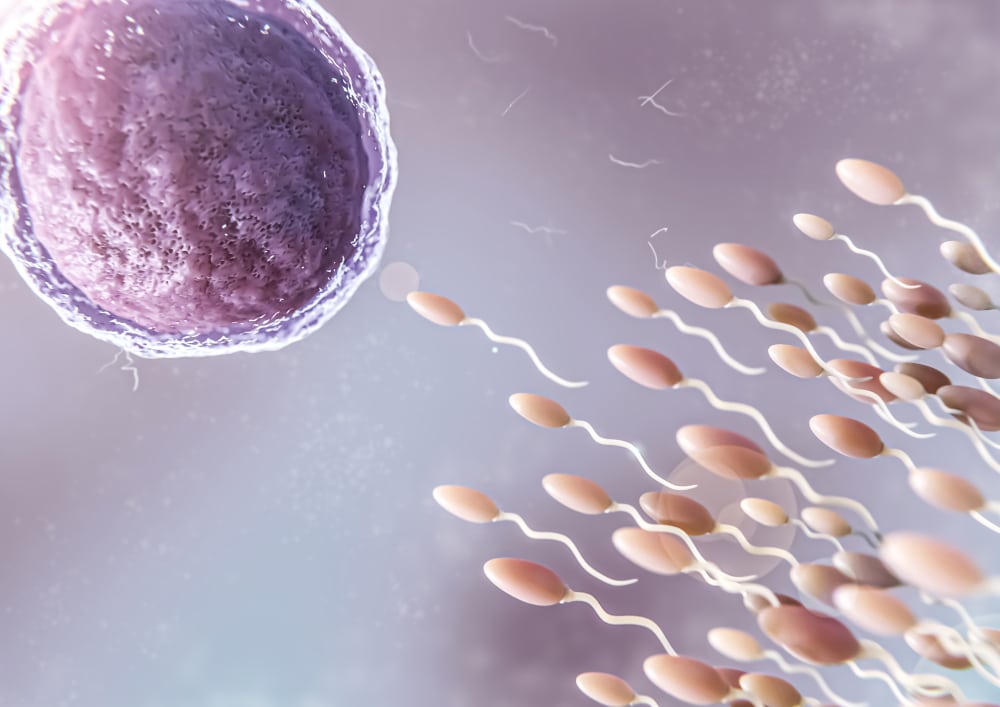
According to a 2023 study published in Nature, “Clinical infertility is the inability of a couple to conceive after 12 months of trying. Male factors are estimated to contribute to 30 to 50 per cent of cases of infertility.” This highlights the importance of recognising that male reproductive health is not limitless. Understanding how age affects sperm quality, testosterone levels, and reproductive outcomes is essential, not just for conception but also for the health of offspring and maternal outcomes.
How does ageing affect male fertility?
The decline in male fertility with age is often more subtle than in women, but it is significant. A comprehensive review conducted in 2001 examined research from 1980 to 1999 to determine the association between male age and semen quality, including volume, sperm concentration, motility, and morphology, as well as fertility outcomes such as pregnancy rates and time to conception.
The review found that “among the methodologically stronger studies, decreases in semen volume of 3–22 per cent, decreases in sperm motility of 3–37 per cent, and decreases in per cent normal sperm of 4–18 per cent were likely when comparing 30-year-old men to 50-year-old men. Most studies examining fertility status suggest a relationship between male age and fertility, but the results are most likely confounded by female partner age.” (sic.)
When studies controlled for female partner age, the effect of male age on fertility became clearer. Men over 50 had 23 to 38 per cent lower pregnancy rates than men under 30. Increased risks for subfertility ranged between 11 and 250 per cent, depending on the study.
Dr Rashmi Niphadkar, fertility specialist at Nova IVF Fertility, Pune, explains that age acts as an independent factor affecting sperm quality. “Older men tend to have a slightly higher DNA fragmentation index and more de novo mutations in their DNA, along with a decline in sperm count, motility, and morphology,” she says. However, she adds that lifestyle factors often amplify these changes. “Smoking, obesity, alcohol, poor diet, and disturbed sleep are powerful modifiers when it comes to sperm health. Age matters, but healthy lifestyle changes can meaningfully improve sperm quality.”
Unlike women, men often do not experience dramatic early symptoms of declining fertility. According to Dr Niphadkar, “Some red flags can include trouble achieving erections or ejaculation, or smaller and softer testes, but these are not always directly linked to fertility. In most cases, the only sign of declining fertility is detected during semen analysis.”
Hormonal changes also play a role. Testosterone, the hormone central to male reproductive health, declines with age. Early research noted that men over 60 had roughly 20 per cent lower testosterone levels, those over 70 had 33 per cent lower, and men above 80 experienced a 50 per cent reduction. Lower testosterone affects libido, erectile function, sperm production, and overall reproductive health.
Addressing a common misconception, Dr Niphadkar clarifies that testosterone therapy is not a treatment for male infertility. “If you provide testosterone externally, it suppresses the body’s natural sperm production. So, we never prescribe testosterone directly for fertility issues,” she explains. Instead, specialists use adjuvant treatments like clomiphene or HCG injections that stimulate the body’s own hormonal response to improve fertility.
“Low testosterone does impact libido, erectile function, and sperm production. But the solution isn’t giving testosterone from outside — it’s about helping the body restore its own balance,” she adds.
At what age does male fertility begin to decline?
According to Dr Niphadkar, the male fertility curve looks quite different from that of women. “In women, we see a sudden cliff where fertility drops rapidly after a certain age. In men, however, it’s a steady, continuous decline,” she explains. The subtle decline usually begins in the mid-thirties, but “the real impact becomes noticeable around 40 to 45 years of age.”
A large study comparing men over 35 with men under 25 found that older men had a 50 per cent lower chance of achieving pregnancy within 12 months. This demonstrates that male fertility, though more gradual than in women, is not immune to age-related decline.
Dr Niphadkar advises that men above 35 who plan to delay childbirth should monitor their fertility regularly. “If you’re over 35 and not yet planning to have a baby, it’s sensible to have your semen tested once a year,” she says.
However, for those actively trying to conceive, she stresses that both partners should get evaluated simultaneously. “We often see women coming in for consultations while their male partners delay testing. It’s important that both get tested at the same time to save crucial time in identifying any issues,” she adds. For men choosing to postpone fatherhood, an annual semen analysis is a simple and proactive way to stay informed about reproductive health.
Male age and offspring health
Male age influences more than just the ability to conceive. Studies show that children born to older fathers are at higher risk for certain conditions, particularly neuropsychiatric disorders. Even when men can conceive at an advanced age, certain risks to offspring increase. Conditions that become more likely in children born to older fathers include schizophrenia, autism, bipolar disorder, and other neurodevelopmental or cognitive challenges such as ADHD or dyslexia.
For example, a study of over 3 lakh men found that fathers over 40 were 5.75 times more likely to have children diagnosed with autism spectrum disorder than younger men, even after controlling for maternal age and socioeconomic factors. Other research indicates that men between 45 and 49 have twice the risk of having children with schizophrenia compared to fathers under 25, while men over 50 face a threefold increase in risk.
Older paternal age may also impact pregnancy outcomes. Research from Columbia University found that women, even when young and healthy, had higher miscarriage rates if their male partner was older. Another study noted that men over 45 had 14 per cent higher likelihood of premature birth, independent of maternal age. Evidence also suggests that paternal age can contribute to preeclampsia, gestational diabetes, and IVF failure. These findings underscore that male reproductive ageing has consequences beyond sperm count. It can directly influence the health of both mother and child.
Dr Niphadkar notes that while the risks are real, they remain relatively small. “Advanced paternal age does cause a modest rise in certain conditions like autism spectrum disorder and schizophrenia,” she explains. The increase, she adds, is progressive rather than abrupt. “After 40 to 45, we start to see a slight but consistent rise in the risk of rare genetic or neurodevelopmental disorders. However, the effect is quite modest and it’s not alarming, but it’s something couples should be aware of when planning pregnancies later in life.”
Expert advice on the ideal age for fatherhood
When it comes to male fertility, timing plays a more subtle role than it does for women, but it still matters. According to Dr Niphadkar, the late twenties to early thirties are considered the “most ideal and optimal age for sperm quality.” During this phase, men generally have the best semen parameters, including sperm motility, count, and morphology, and the lowest chances of DNA fragmentation.
However, she adds that fatherhood in the late thirties is still quite common and “perfectly fine” in most cases. “It’s only when the age goes beyond 40 that couples should consider preconception counselling and genetic testing,” she explains. This helps identify any potential hereditary or chromosomal concerns before conception and ensures both partners are in optimal health for pregnancy.
Dr Niphadkar emphasises that lifestyle choices significantly affect fertility, sometimes even more than age itself. “If you’re someone who smokes, the first and most impactful change is to quit smoking completely,” she says. Reducing alcohol intake and maintaining a healthy weight are the next crucial steps. Obesity, she notes, has a strong correlation with reduced sperm quality and hormonal imbalance.
A balanced diet also plays a vital role. “Swapping processed food for nutritious, antioxidant-rich meals can do wonders for sperm vitality,” she says. Foods high in vitamins C and E, zinc, selenium, and omega-3 fatty acids are particularly beneficial for maintaining healthy sperm function.
When it comes to supplements, Dr Niphadkar advises caution. “There are supplements like CoQ10, L-carnitine, zinc, and selenium that can support sperm health, but taking them without medical guidance is like shooting in the dark,” she cautions. She typically recommends such supplements only two to three months before conception, under a doctor’s supervision. Overuse or incorrect dosage, she warns, can actually harm sperm quality.
Finally, she notes that managing underlying health conditions such as diabetes, hypertension, or metabolic disorders is key. “Getting these issues under control is not just a win for your overall health, but also for your sperm health,” she adds.
Also read:FACT CHECK: Are gel nail paint manicures harming your fertility?
(Do you have a health-related claim that you would like us to fact-check? Send it to us, and we will fact-check it for you! You can send it on WhatsApp at +91-9311223141, mail us at hello@firstcheck.in, or click here to submit it online)










