India faces alarming rise in gastric cancer without H. pylori prevention
A new Nature Medicine study warns that China and India could together see 6.5 million gastric cancer cases in future generations without H. pylori screening
Author
Author
- admin / 7 months

- 0
- 3 min read
Author
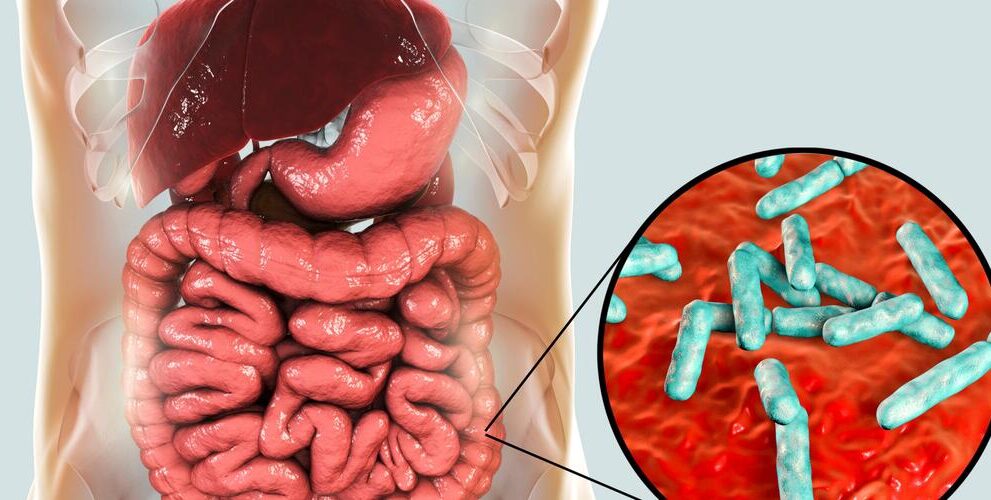
India could see a dramatic rise in gastric cancer among those born between 2008 and 2017 unless it takes urgent action to eradicate Helicobacter pylori, a new study warns.
The research, led by Jin Young Park and colleagues and published this week in Nature Medicine, estimates that “15.6 million (95% uncertainty interval 14.0–17.3 million) lifetime gastric cancer cases are expected within these birth cohorts” across 185 countries, and that roughly 76% of those cases are directly attributable to H. pylori infection.
In Asia, the burden is most heavily concentrated. The study projects “more than 10.6 million cases (68% of all cases)” will occur on the continent, with India and China together making up about 6.5 million of those cases. That number is staggering when compared to current rates — driven by demographic shifts and increasing infection trends.
“Among the expected gastric cancer cases, approximately 76% are attributable to H. pylori infection globally, with 8.0 million gastric cancer cases in Asia attributable to the bacteria,” the research says.
In India, H. pylori infection is widespread but gastric cancer rates have been lower than in East Asia since a long time.
The researchers describe this as the “Indian enigma.”
India has a high prevalence of H. pylori infection but relatively low rates of gastric cancer, attributed to variables like diet, genetic resistance and specific bacterial strains.
Yet the study’s predictive model suggests that cohort trends may overcome these protective factors in the coming decades.
“About two-fifths (42%) or 6.5 million (95% UI 6.1–6.9 million) new cases among these cohorts will occur in China and India alone,” the study states.
The researchers reinforced the potential of early intervention: “gastric cancer is largely preventable,” they write, and call for “population-based H. pylori screen-and-treat strategies”.
The study notes that “up to 75% of future gastric cancer cases could be prevented” by such programs.
In India, the idea of community-wide antibiotic and proton pump inhibitor treatment which has been standard in trials in East Asia, has not been widely implemented. Most current screening in India focuses on symptomatic patients via endoscopy, not broader eradication efforts. The new findings strengthen the case for shifting toward preventative population health models.
Health officials say that a nationwide rollout may still be feasible. While antibiotic resistance and logistical hurdles remain concerns, the IARC team pointed out that even “programs with 80–90% effectiveness would still prevent 60–68% of cases,” making them cost-effective public health tools.
The Nature Medicine study’s focus on birth cohorts, rather than current incidence rates, gives fresh urgency to the issue. “Shifting from a traditional cross-sectional lens to a birth-cohort approach can aid policymakers to design and implement effective and timely prevention programmes,” the researchers conclude.
In India’s fight against cancer, targeting a silent bacterial infection could become one of the most impactful strategies. Without such action, a generation born between 2008 and 2017 could bear a growing weight of disease, one that may have been largely preventable.
Also read: Can you protect yourself from cancer-causing plastic chemicals?
Do you have a health-related claim that you would like us to fact-check? Send it to us, and we will fact-check it for you! You can send it on WhatsApp at +91-9311223141, mail us at hello@firstcheck.in, or click here to submit it online.










