Latest
Rise of telemedicine: Bridging healthcare’s digital divide
From rural hills to urban homes, virtual consultations are breaking healthcare barriers
Author
Author
- admin / 5 months

- 0
- 10 min read

Author
Telemedicine has emerged as a game-changer in the field of health, enabling remote health consultations across geographical barriers. This ensures a more inclusive, patient-centric and efficient approach to health care.
At its heart, telemedicine involves receiving medical and health care over the internet using a computer, smartphone, tablet, and other such smart technological gadgets. Doctors diagnose and treat patients remotely through video calls, phone consultations, and online messaging.
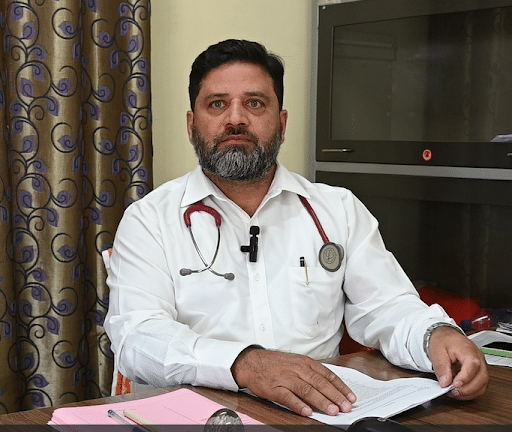
“Telemedicine bridges geographical gaps,” says Dr. Abid Ahmed Sofi, an emergency specialist, currently posted as Medical officer and Incharge Clinical establishment at Central University of Kashmir. “It’s a game-changer for patients who live in underserved or rural areas.”
The COVID-19 pandemic accelerated the adoption of telemedicine, but its benefits extend beyond the crisis. Telemedicine, according to Dr. Abid, is here to stay.
“The pandemic highlighted its potential, but even after things returned to normal, telemedicine continues to play a significant role in healthcare,” he says.
The Rise of Telemedicine
The concept of ‘telemedicine’ originated over 50 years ago when NASA developed telehealth services for astronauts on long-duration missions. While ‘telehealth’ and ‘telemedicine’ are sometimes used interchangeably, there are subtle differences between the two. The term “telehealth” encompasses a broad spectrum of services, which include establishing connections between various providers such as pharmacies and labs, delivering remote training, coordinating staff members like home health aides, and facilitating the management of remote admissions.
The earliest published record of telemedicine dates back to the early 20th century, when ECG data was transmitted over the phone. Things like the telegraph and telephone were key to making telemedicine what it is today. Phones, especially emergency numbers like ‘911,’ made it quicker to get medical help.
A magazine cover in 1924 showed a person with a TV and microphone talking to a doctor. It was a cool idea, but TVs weren’t common yet. The first live video consultation happened in 1959 at the University of Nebraska, when they used telemedicine for neurological exams. NASA used it during the 1985 Mexico City earthquake and the 1988 Soviet Armenia earthquake, when traditional communication was down. They used satellite technology, which was a big deal then. In 1997, NASA set up MITAC (Medical Informatics and Technology Applications Consortium) at Yale University, which got private companies involved in public health through telemedicine.
The Plague of Long Queues and Waiting Times
One of the most pressing issues in traditional healthcare settings has been the perennial problem of long queues and waiting times. In a world where time is of the essence, these delays can not only exacerbate a patient’s physical condition but also their mental and emotional well-being. Telemedicine has come as a beacon of hope, effectively tackling this long-standing challenge. With the ability to consult a healthcare provider remotely, patients are no longer bound by the constraints of physical presence, eliminating the need to spend hours in crowded waiting rooms. This newfound freedom not only reduces stress on patients but also optimizes the allocation of medical resources, enabling healthcare facilities to serve a greater number of individuals.
“Telemedicine allows not only patients but doctors as well to access medical advice, consultations, and even prescriptions remotely,” Dr. Shiny Rashid, General Physician at Primary Health centre Zakura, said. “By utilizing technology, we can bridge the gap in healthcare access, particularly for individuals in rural or underserved areas. Telemedicine reduces wait times, offers convenience, and improves overall healthcare outcomes.”

When it comes to medical emergencies or urgent healthcare needs, every minute counts. Telemedicine demonstrates its true power by providing immediate treatment options to patients, regardless of their location. Consider a scenario where a patient in a remote rural area is grappling with a sudden health crisis. In the absence of nearby medical facilities, telemedicine emerges as a lifeline, connecting the patient with a qualified medical professional who can assess the situation in real time and provide guidance on the necessary steps. This capacity for instantaneous medical attention has the potential to save lives and prevent the escalation of critical conditions.
Empowering Patients Through Accessibility
Inclusion lies at the heart of the telemedicine revolution. The traditional healthcare model often overlooked individuals who resided in rural or underserved areas, where access to medical care was a luxury. Telemedicine disrupts this disparity by democratizing healthcare access. Patients living in remote regions can now tap into a global network of doctors and specialists, transcending geographic barriers and ensuring that quality medical advice is never out of reach. This newfound accessibility empowers patients to take charge of their health, fostering a sense of agency and well-being.
Enhancing Doctor-Patient Collaboration
Contrary to concerns that telemedicine might hinder the doctor-patient relationship, this innovative approach has been proven to enhance collaboration between healthcare providers and their patients. In a virtual consultation, patients often feel more at ease, facilitating open and transparent communication about their symptoms and concerns. Doctors, on the other hand, gain insights into the patient’s environment and lifestyle, enabling them to provide personalized recommendations that extend beyond mere prescriptions. This strengthened connection fosters a holistic approach to healthcare where patients are active participants in their wellness journey.
Telemedicine in India
India, with over 1.4 billion people, faces a big challenge in making sure healthcare reaches everyone fairly. As per research published in the National Center for Biotechnology Information, WHO recommends a doctor-population ratio of 1:1000 while the doctor-population ratio in India was only 0.62:1000. Even though India has now surpassed the WHO recommended guideline, Telemedicine still has an important role to play. Most of the healthcare resources, including 75% of doctors, have been centered in cities and towns, leaving out rural areas where nearly 69% of the population lives. This makes fair healthcare distribution a recurring concern in public health management.
In 2001, ISRO (Indian Space Research Organization) started telemedicine in India by connecting Chennai’s Apollo Hospital with a rural hospital in Andhra Pradesh. ISRO, along with other government departments, has played a key role in developing telemedicine services.
The Indian government has launched projects to consolidate public health data and provide easy access. They’ve set up guidelines and a National Telemedicine Task Force. India has also initiated international projects like the Pan-African eNetwork Project and the SAARC Telemedicine Network, making a mark on the global stage. Some of the Digital Healthcare Infrastructure set up by India include – Ayushman Bharat Digital Mission, Telemedicine and e-Sanjeevani, U-Win Portal, Aarogya Setu App, e-Hospital, National Tele Mental Health Programme.
A World Economic Forum report titled ‘India Can Be a Global Pathfinder in Digital Health,’ released on January 15, 2024, highlights how India’s digital health initiatives are paving the way for the country to emerge as a global leader in health technology.
Successful examples of telemedicine in India include mammography services in Delhi, oncology services in Trivandrum, and surgical services in various institutions. Telemedicine is also used during large gatherings, like the Maha Kumbh Mela in Uttar Pradesh, to provide medical care when needed.
The private sector has shown keen interest in telemedicine, with major players like Narayana Hrudayalaya and Apollo Telemedicine Enterprises partnering with government organizations like ISRO to use updated technology for public health.
ISRO’s telemedicine network has expanded, connecting 45 rural hospitals and 15 super specialty hospitals, even reaching remote areas like the Andaman and Nicobar Islands and Jammu and Kashmir’s hilly regions.
Telemedicine in India falls under the jurisdiction of the Ministry of Health and Family Welfare and the Department of Information Technology. The Ministry’s Telemedicine Division has set up a National Telemedicine Portal for initiatives like the National Medical College Network and the National Rural Telemedicine Network.
To ensure secure data transmission, the ministry developed Electronic Health Records (EHR) standards in 2013, which were updated in 2016. Telemedicine isn’t limited to modern medicine; the National Rural AYUSH Telemedicine Network promotes traditional healing through telemedicine.
ISRO introduced Village Resource Centers (VRCs) to provide various services, including tele-education and telemedicine, linking rural areas to specialist hospitals. Over 500 VRCs have been established across India.
AROGYASREE is another initiative, integrating multiple hospitals, mobile medical specialists, and rural clinics. It’s a project by the Indian Council of Medical Research (ICMR), with collaboration from German scientists working on an ECG jacket for continuous patient monitoring without hospitalization.
Challenges in the way of Telemedicine
While the inclusion of telemedicine in contemporary medicine offers remarkable benefits, it is not without its challenges. One of the primary concerns revolves around data security and patient privacy. Transmitting sensitive medical information over digital platforms demands robust cybersecurity measures to safeguard patient data from unauthorized access. Additionally, ensuring that patients from diverse backgrounds have access to the necessary technology and connectivity poses a hurdle in achieving universal telemedicine adoption. Addressing these challenges requires collaborative efforts from healthcare providers, technology developers, and policymakers.
“Majority of the population in India is not well equipped or well versed with technology, which is a major hurdle in telemedicine approach,” Dr. Shiny said.
Dr. Abid highlighted the need for possession of a smartphone and a stable internet connection for anyone to avail telemedicine service.
“But for many in rural areas and those from low-income backgrounds, having both is a big challenge,” he said. “This makes it hard for them to benefit from telemedicine, limiting its reach and impact where it’s needed the most.”
Dr. Nasir Shaheen, demonstrator and tutor at the Department of Pharmacology, Government Medical College, Srinagar said that it was difficult to diagnose any disease in online mode.
“There are different fluids in the body which are released in response to infections in the body,” he explained. “So, diagnosing such issues in absence of clinical examinations pose a challenge.”
Shaping the Future of Healthcare
As telemedicine gains momentum, its potential extends beyond individual patient care. Remote consultations can be leveraged for specialized medical training, allowing doctors to learn from experts across the globe without the constraints of travel. Moreover, telemedicine can contribute significantly to public health initiatives by enabling the timely dissemination of information during disease outbreaks or natural disasters. The integration of telemedicine with wearable health technology holds the promise of continuous monitoring, enabling doctors to proactively address health issues before they escalate.

The inclusion of telemedicine in contemporary medicine is steering the healthcare industry toward a future characterized by inclusivity, efficiency, and immediate access to treatment. By dismantling the barriers of distance and time, telemedicine is not only reducing long queues and waiting times but also providing patients with timely medical attention, especially during emergencies. This technological advancement empowers patients, enhances doctor-patient collaboration, and promises to reshape healthcare delivery on a global scale.
As the world embraces this transformative shift, it is imperative for healthcare stakeholders to navigate challenges and seize the opportunities presented by telemedicine. By fostering a secure and accessible telemedicine ecosystem, we can collectively pave the way for a healthcare landscape that truly puts patients at the center, regardless of their location or circumstances. The journey toward a more inclusive and efficient healthcare system is well underway, with telemedicine as its steadfast compass, guiding us toward a healthier and more interconnected future.
Also read: https: FACT CHECK: Is paracetamol really the world’s most dangerous medicine?
(Do you have a health-related claim that you would like us to fact-check? Send it to us, and we will fact-check it for you! You can send it on WhatsApp at +91-9311223141, mail us at hello@firstcheck.in, or click here to submit it online)









